This post contains affiliate links. Please see our disclosure policy.
Exploring the 10 most common menopause symptoms will help you understand where potential symptoms may be coming from, and how you can take back control of your life during this phase!
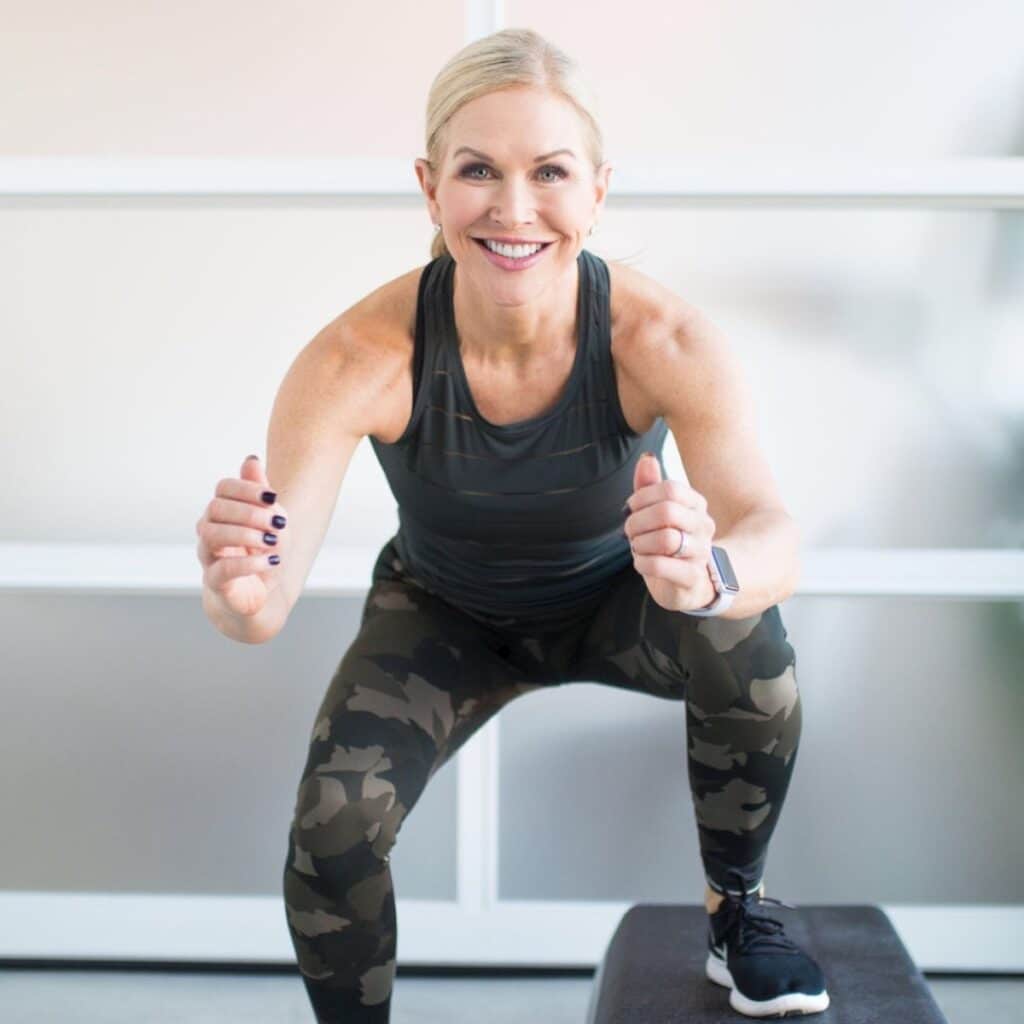
Menopause is a significant phase in every woman’s life, marking the end of her reproductive years. As a certified fitness trainer and health coach who has navigated these changes myself, I understand the challenges you’re facing.
At 48 years old, when perimenopause set in for me, I was uneducated and clueless how to handle these symptoms. Now, at 59 years old, I’ve been through it all. I have spent hours learning and researching and I now know why these menopausal symptoms occur and the best ways to naturally handle them.
I talk to thousands of midlife women as part of my job who are going through this transition and experiencing these symptoms, and it’s important to remember you are not alone.
And I like to say “aging is inevitable but suffering is not.” Pretty much every woman will experience some, (if not all) of these symptoms, and more solutions are now available as menopause becomes a more openly discussed topic.
I’m going to break down the ten most common menopause symptoms and the best treatment options to effectively manage these changes. Knowledge is power, and when you’re armed with these tips, it makes navigating menopause in daily life a little bit easier.
Save This Article To Read Later
The Phases of Menopause
Perimenopause are the years leading up to menopause when your sex hormones (primarily progesterone, and estrogen) begin to fluctuate indicating the natural decline and eventual end of ovarian function within your menstrual cycle.
The length of this stage is impossible to diagnose. Each woman’s experience is different.
Menopause is just actually one day. It’s the day on the calendar that marks the absence of menstrual periods for 12 consecutive months. It typically occurs between ages 45 and 55.
Post menopause are the years that follow for the rest of your life.
Symptoms typically start in perimenopause and don’t necessarily go away once you are in post menopause. Many of them linger.
Let’s talk about the 10 most common symptoms (believe me, there are about 50 more) and how to deal with them.
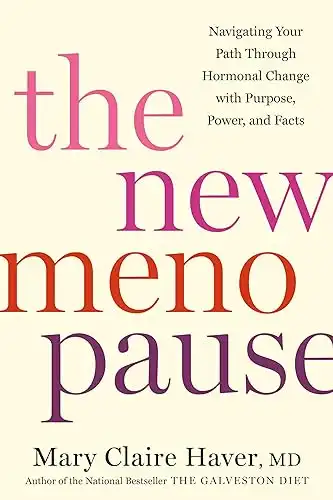
I want to mention that all these symptoms are discussed in The New Menopause Book by Dr. Mary Claire Haver. Chapter 10 is a full tool kit for menopause symptoms and is filled with more details for each of these traits. This book is an amazing resource that I have read many times, highlighted paragraphs and use as a trusted resource. I suggest every woman entering perimenopause reads this book.
1. Hot Flashes
Hot flashes are sudden feelings of warmth, often intense, that spread over the body. They commonly start in the upper body and face and can spread over your whole body instantaneously. You will notice a change in your body temperature, even feeling like your body is on fire.
Why Do Hot Flashes Happen?
Fluctuating hormone levels (less estrogen) affect the body’s temperature regulation. Hot flashes come on very quickly.
How to Deal With Hot Flashes:
- Stay Cool: Wear lightweight clothing and keep your environment cool. Dress in layers (try my favorite Lululemon lookalikes) so you can peel off a few if needed.
- Hydrate: Stay hydrated by drinking plenty of water. Use my tips for drinking more water to get inspiration!
- Diet & Lifestyle: Eating healthy and eliminating processed foods can help. Avoid spicy foods, caffeine, and alcohol which can trigger hot flashes.
- Relaxation Techniques: Practice deep breathing exercises at the onset of hot flashes. Also, for overall stress reduction try meditation.
- Cooling Necklaces: A friend tipped me off to these Hot Girl Pearls. She warned me they are large (like Wilma Flintstone size), but they work. I also love these Nano-Ice Cooling necklaces which come in a variety of colors.
2. Night Sweats
Night sweats are different than hot flashes. Think of them as hot flashes on steroids that occur during sleep, causing excessive sweating. Basically, you wake up and your pajamas and sheets are soaking wet.
I went from sleeping in sweatpants and socks to wearing a tank top and shorts with a fan blowing on my face even in the middle of winter.
What Causes Night Sweats?
Again, hormonal fluctuations, particularly decreased estrogen levels, interfere with the body’s heat regulation.
How To Deal With Night Sweats:
- Bedroom Environment: Keep your bedroom cool and well-ventilated. Use a ceiling fan. I also put a fan facing me on my nightstand.
- Light Bedding: Use lightweight blankets and moisture-wicking pajamas.
- Hydration: Drink plenty of fluids throughout the day.
3. Joint Pain
Many women experience menopause joint pain and stiffness. I had no idea this was a symptom of perimenopause and I had hip pain for months thinking I had pulled a muscle. Finally I was tipped off that this could be normal in perimenopause.
This issue often goes undiagnosed but it can be a real problem.
Why Does Menopause Joint Pain Happen?
The decline in estrogen can cause inflammation and pain in the joints.
How To Deal With Menopause Joint Pain:
- Stay Active: Regular workouts and mobility exercises help keep joints flexible. Joints are where two bones come together and keeping them naturally lubricated through consistent movement helps. My motto is “motion is lotion”.
- Diet: Eat a healthy diet rich in anti-inflammatory foods like fatty fish, nuts, and leafy greens.
- Supplements: Consider Omega-3 supplements for joint health.
4. Mood Swings
Mood swings are sudden and intense changes in emotional state, often without any apparent reason. Think irritability, depression, more anxiety than usual. One minute you are fine, the next you are sobbing at a sappy commercial.
You feel like you aren’t controlling your own emotions or mood changes.
What Causes Menopausal Mood Swings?
Hormonal imbalances can impact brain chemicals that regulate mood. And, if you are sleep deprived (another one of our 10 common symptoms) your mood swings are worse.
How to Handle Mood Swings:
- Mindfulness & Meditation: Practice stress-relief techniques.
- Healthy Lifestyle: Regular exercise and balanced nutrition can stabilize mood. Make sure you are getting your vitamins and minerals and needed supplements.
- Social Support: Engage with friends, family, or support groups. I am not a mental health professional but if these feelings become unbearable, please seek the help of a therapist, psychologist, and your doctor.
5. Menopausal Weight Gain
Menopause related weight gain is incredibly common and often accumulates around the abdomen. I’ve put together my top tips for getting rid of menopause belly fat.
What Causes Menopausal Weight Gain?
A slowing metabolism and hormonal changes during menopause contribute to weight gain.
How to Handle Menopausal Weight Gain:
- Balanced Diet: Focus on whole foods and reduce processed foods. Eat more protein and fiber. Get rid of chemicals, fake food coloring and additives which cause inflammation.
- Regular Exercise: Incorporate both cardio workouts and strength training. If you are not strength training and you are over 50, now is the time. Muscle is the key to aging and staying strong and keeping your metabolism energized. Check out the five benefits of HIIT exercise during menopause if you don’t believe me!
- Portion Control: Be mindful of your portion sizes. Calories do matter.
6. Poor Sleep
Sleep problems can look like difficulty falling asleep or staying asleep, often leading to overall fatigue. If you’re struggling with a consistent nighttime routine, check out my science-backed tips for getting better sleep.
What Causes Poor Sleep in Menopause?
Hormonal changes can disrupt your sleep patterns. For me, I started waking up between 2 and 3 am in perimenopause and couldn’t fall back to sleep.
How to Improve Poor Sleep:
- Sleep Routine: Establish a consistent sleep schedule. I had to get rid of my phone in bed!
- Caffeine Intake: Avoid caffeine. This was key for me was not having any after lunch.
- Sleeping Environment: Create a cool, dark, and quiet sleeping space.
- Supplements: There are many natural supplements that contain melatonin, magnesium, and other ingredients to help keep you fall and stay asleep.
7. Brain Fog
Many women experience brain fog as a common symptom of menopause. It’s recognized as forgetfulness or difficulty concentrating. It can also look like having a hard time remembering words or recalling what you just did or why you walked into a room.
What Causes Brain Fog
Hormonal shifts can affect cognitive function. As estrogen drops, your receptors may not be triggering well and your lack of recall, concentration and focus can worry you.
How To Deal With Brain Fog:
- Mental Exercises: Engage in activities that challenge your brain. Play games, read daily, learn new things.
- Stay Organized: Use planners and reminders.
- Healthy Lifestyle: Maintain a balanced diet and regular physical activity.
- Stay Socially Connected: Connect with friends, family. Don’t isolate yourself.
8. Loss of Libido
During menopause many women experience a loss of libido, or decrease in sexual function. All of the sudden you may have a lack of interest in sex, vaginal dryness, pain during sex and these issues can lead to feeling frustrated and confused.
What Causes a Loss of Libido During Menopause?
Lower estrogen levels can reduce blood flow to the genital area and decrease arousal. This is a complex subject and there are a few things you can do on your own but reaching out to your health care provider to talk about your menopausal transition for more strategies is encouraged.
How To Deal With Loss of Libido:
- Open Communication: Talk with your partner about your needs and concerns.
- Lubricants: Over-the-counter vaginal moisturizers and water-based lubricants can help alleviate vaginal dryness and discomfort during sex.
- Consult a Doctor: Seek advice on possible treatments.
9. Skin Changes
Many women experience noticeable changes in skin texture coupled with the onset of wrinkles, dry patches, itchy skin, and slow healing of wounds. This one is a doozy.
Many women complain of crepey arms, legs, and necks in particular.
What Causes Skin Changes During Menopause?
Once again, the decline of estrogen is the culprit because it causes less blood flow to your skin. Menopause also brings on an accelerated loss of collagen and elastin.
How To Deal With Skin Changes:
- Diet and Supplements: Make sure to take adequate vitamin D. Collagen supplements can be helpful also. I use collagen peptides every day.
- Topical Moisturizers: Use quality moisturizers with ingredients like hyaluronic acid to hydrate the skin. Use topical retinoids and Beta hydroxy acids to improve texture.
- Strength Train: You can’t eliminate crepey skin but by building muscle, it certainly looks better.
- Stay Hydrated: Drink plenty of fluids throughout the day.
- Skin Treatments: Talk to your dermatologist or a medispa about options to reach your skin goals.
- Lifestyle Changes: Wear a clean sunscreen. Wear UV protective clothing and avoid peak sun hours.
10. Migraine Headaches
Migraines and headaches are a common menopause symptom. Many women experience frequent or severe headaches that may be new or worsening.
A migraine is a specific type of headache that is often characterized by throbbing pain on one side of the head.
What Causes Migraines During Menopause?
Hormonal fluctuations can trigger headaches or migraines. For me migraines started in post menopause. Out of the blue, just above my left eye would throb with pain. And if I had a glass of wine, it was debilitating.
Prior to this I would drink wine occasionally and truly never had a headache in my adult life I could remember.
How To Improve Menopausal Migraines or Headaches?
- Hydration: Drink plenty of water.
- Alcohol Intake: Reduce alcohol consumption. This was key for me.
- Over-the-Counter Pain Relief: Use medications like Advil as needed. I am not a big fan of OTC pain killers, but Advil and Excedrin make a difference.
- Professional Advice: If headaches persist, consult a healthcare provider.
Another Solution: Hormone Replacement Therapy (HRT)
As you noticed, all these symptoms are brought on by the natural decline and fluctuation of your sex hormones, estrogen in particular. (Hormones in general are chemical messengers that tell your cells what to do.)
Declining estrogen and progesterone create significant changes in the physiology of your body. Estrogen in particular has a protective effect on so many systems in the body.
Using HRT can be super beneficial with helping to manage these symptoms as well as many others. There has been so many misconceptions about HRT in the last decades and much of it can be traced back to the Women’s Health Initiative Studies in 2002.
There are so many options for HRT but keep in mind it is not for everybody.
I have learned from reading Dr Mary Clare Havers Book:
- You should not take estrogen alone. It’s important to also take progesterone to maintain a healthy ratio.
- There are so many possible forms and no right answer for all women. Oral, transdermal, pellets, and other options are available. You must find a health care provider willing to evaluate you and prescribe the right option for you.
- You need to be flexible. You may have to try out a few options and adjust doses as you see how it works for you.
I personally take bioidentical estrogen and progesterone. It’s primarily for the protective and anti-inflammatory properties for my heart and body.
I encourage you to find a provider or doctor in your area. Dr Mary Claire Haver has information as to how to approach your healthcare provider about hormone therapy.
Remember, while these healthy conditions and symptoms are common, everyone’s experience is unique. Always consult with your doctor to discuss any concerns or symptoms you may be experiencing that are impacting your quality of life.
You are not alone, and with the right strategies, you can navigate menopause with confidence and grace.
It’s time to become better educated about your options for HRT and how to seek out a health care professional for help!
| Product Image | Product Name | Primary Button |
|---|---|---|


These sound awesome and way too easy! Curious though…no adding water/oil/milk/egg to either of the two recipes?
Thanks!
Not helpfull, I’ve tried everything for the last 15 years am still having atrocious day and night sweats
Sticky skin feeling help?Renee
I wish I had looked for additional articles regarding perimenopause and/or menopause and sticky skin after last summer, then maybe I could have helped others! Many people think that sticky skin is sticky sweat, but it’s not. I have sticky skin after washing my hands in cold water, so sweat is not the issue! I have not gone to traditional doctors in a long time due to trust issues and the lack of bedside manners with most so I don’t know if HRT can help, but I am considering it. What I have found to give me some relief in the mean time is using supplements. If you can find a holistic/homeopathic practitioner, maybe they can help determine what you need. We think that for me, it’s been Core Milk Thistle but we are not certain since that supplement is for liver support (my liver is healthy by the way, we check this all the time). I do find when I am taking it, my sticky skin can decrease. And I shower with Neutrogena’s “Body Clear Body Wash”, it has salicylic acid, which tends to help with some relief.
Try sage tea